Nutrients for blood glucose control: a review and clinical guide
Nutrients for blood glucose control: a review and clinical guide
Posted on Tue, 24 Sep 13

Illnesses related to poor blood glucose control and insulin resistance are amongst the most commonly encountered in clinical practice. Although type-2 diabetes, which affects more than one in 20 people (1), is the most apparent example there are a host of other common insulin resistance related illnesses including obesity, hyperlipidaemia, hypertension, dermatological disorders (e.g. acne, skin tags, and acanthosis nigricans) and polycystic ovary syndrome (PCOS) (2).
Dietary change, exercise, behavioral changes and medication are typically the first-line treatment for improving blood glucose control however there are concerns about the real-world benefits and potential side effects of conventional medications (3,4). Nutritional supplements are receiving increasing interest as a viable treatment option and in some cases there is rigorous evidence that certain supplements could be included in standard care for improving blood glucose control (5).
Because the effectiveness of nutritional interventions is influenced by factors such as dietary intake and variations in requirements and metabolism it is unlikely that a “one size fits all” prescription is appropriate. An individualized prescription based on the best available evidence would therefore be a logical approach to improving blood glucose control with nutritional supplements. This article summarizes a selection of nutritional supplements with compelling evidence for clinical efficacy and concludes with a summary and guide for developing a personalized prescription (table 1).
Cinnamon
The culinary spice cinnamon was found in a meta-analysis of 6 clinical studies to improve blood glucose control with statistically significant improvements in glycosylated haemoglobin A1c (HbA1c) and fasting blood glucose (FBG) in studies of up to 4 months duration (6). A more recent meta-analysis of 10 clinical studies however found inconsistent evidence for cinnamon (7). Compared to medications the reduction in fasting glucose from cinnamon (–24.59 mg/dL) was lower than metformin (–58 mg/dL) and superior to sitagliptin (–16 to –21 mg/dL). Cinnamon is promising but it appears better quality research is needed to clarify its clinical use (8).
Chromium
Chromium has been subject to several clinical trials but these have generally produced inconsistent findings with some showing benefit while others do not (9). A review of clinical studies suggested that individuals with more severe insulin resistance might have a better response to chromium supplementation; specifically individuals with type-2 diabetes and marked elevations in fasting glucose and HbA1c (10).
Pycnogenol
Pycnogenol is a standardized extract of French maritime pine bark composed of procyanidins and phenolic acids. One open label preliminary study and two randomized controlled trials (RCTs) have demonstrated the ability of pycnogenol to improve blood glucose control in diabetics (11-13). The RCTs also found benefit for cardiovascular risk factors suggesting pycnogenol may be particularly useful for reducing associated cardiovascular risk (14).
Lipoic acid
Both intravenous and oral administration lipoic acid has been studied in type-2 diabetics and it appears the effects or oral supplementation are modest, with improvements insulin sensitivity following supplementation typically less than 20% (15). However lipoic acid is a potent anti-oxidant and improves nerve function making it a potentially useful supplement for managing complications of elevated blood glucose and oxidative stress including vascular disease and neuropathy (16,17).
Sweet potato
A particular sweet potato (Ipomoea batatas) extract has been used as a dietary supplement for type-2 diabetes in a number of studies. A systematic review of 3 clinical trials found a statistically significant improvement in HbA1c at three to five months with 4 grams a day of a sweet potato dietary supplement compared to placebo (18).
Inositol
Several studies have found myo-inositol to be very effective for the treatment of PCOS, primarily due to its ability to improve insulin sensitivity (19). Emerging evidence also suggests that myo-inositol may be effective the treatment of other disorders related to insulin resistance including gestational diabetes mellitus, metabolic syndrome as well as the management of diabetic complications (20).
Magnesium
There is very strong evidence to show that low dietary magnesium intake is associated with risk of type-2 diabetes, in a dose-response manner (21). Furthermore a meta-analysis of 9 clinical studies of magnesium supplementation in type-2 diabetes found consistent benefits for reducing plasma fasting glucose levels and raising HDL cholesterol at a median dose of 360 mg per day for 4-16 weeks (22).
Vitamin D
Vitamin D deficiency is an emerging risk factor for insulin resistance, type-2 diabetes, metabolic syndrome and PCOS (23,24). Various lines of evidence suggest that the association between vitamin D deficiency and insulin resistance may be causal (25). However clinical studies examining the effect of vitamin D supplementation on blood glucose, insulin resistance and HbA1c have not shown consistent benefit (26). Despite this it should be noted that studies so far have been poorly designed and not accounted for important factors such as baseline vitamin D status or provision of an adequate dose to correct deficiency, so further research is needed before firm conclusions can be made (27).
Table 1: Summary and guide for developing a personalized prescription
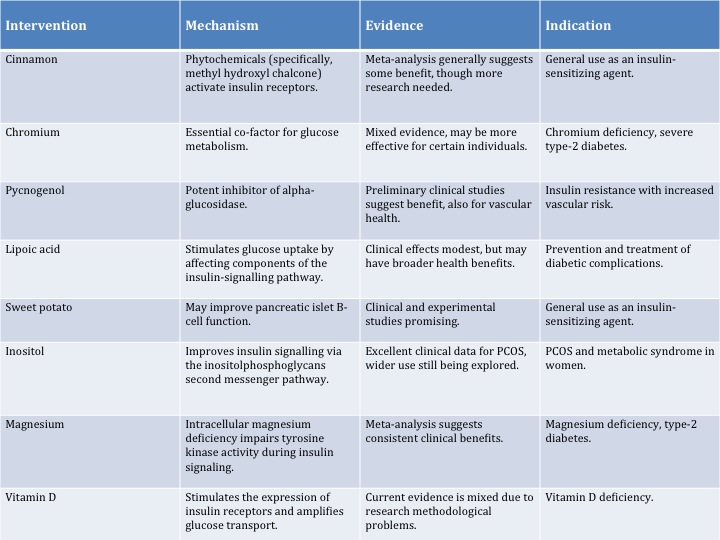
Nutritional supplements in practice
The use of safe, relatively low-cost nutritional supplements should be considered in the management of insulin resistance, type-2 diabetes, metabolic syndrome and PCOS due to their ability to improve blood glucose regulation and insulin signaling (see image 1).
Image1: Nutritional supplements and the insulin signaling cascade.
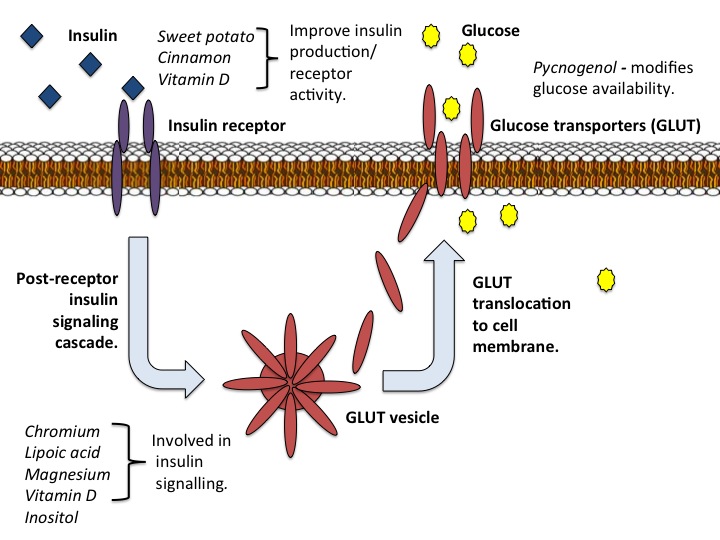
Supplements such as cinnamon and sweet potato could be used as general insulin-sensitizing agents in addition to dietary and lifestyle changes. Lipoic acid appears to have wider reaching benefits for preventing complications of elevated blood glucose while myo-inositol is effective for women with PCOS. The identification and correction of deficiencies in chromium, magnesium and vitamin D is likely to improve blood glucose and have a number of general health benefits.
References:
1. Diabetes UK. Key statistics on diabetes; Diabetes in the UK April 2012.
2. Lee T, Dugoua JJ. Nutritional supplements and their effect on glucose control. Curr Diab Rep. 2011 Apr;11(2):142-8.
3. Cordain L, Eades MR, Eades MD. Hyperinsulinemic diseases of civilization: more than just Syndrome X. Comp Biochem Physiol A Mol Integr Physiol. 2003 Sep;136(1):95-112.
4. Rao AD, Kuhadiya N, Reynolds K, Fonseca VA. Is the combination of sulfonylureas and metformin associated with an increased risk of cardiovascular disease or all-cause mortality?: a meta-analysis of observational studies. Diabetes Care. 2008 Aug;31(8):1672-8.
5. Lipscombe LL. Thiazolidinediones: do harms outweigh benefits? CMAJ. 2009 Jan 6;180(1):16-7.
6. Akilen R, Tsiami A, Devendra D, Robinson N. Cinnamon in glycaemic control: Systematic review and meta analysis. Clin Nutr. 2012 Oct;31(5):609-15.
7. Allen RW, Schwartzman E, Baker WL, Coleman CI, Phung OJ. Cinnamon use in type 2 diabetes: an updated systematic review and meta-analysis. Ann Fam Med. 2013 Sep-Oct;11(5):452-9.
8. Rafehi H, Ververis K, Karagiannis TC. Controversies surrounding the clinical potential of cinnamon for the management of diabetes. Diabetes Obes Metab. 2012 Jun;14(6):493-9.
9. Hua Y, Clark S, Ren J, Sreejayan N. Molecular mechanisms of chromium in alleviating insulin resistance. J Nutr Biochem. 2012 Apr;23(4):313-9.
10. Wang ZQ, Cefalu WT. Current concepts about chromium supplementation in type 2 diabetes and insulin resistance. Curr Diab Rep. 2010 Apr;10(2):145-51. doi: 10.1007/s11892-010-0097-3.
11. Liu X, Wei J, Tan F, Zhou S, Würthwein G, Rohdewald P. Antidiabetic effect of Pycnogenol French maritime pine bark extract in patients with diabetes type II. Life Sci. 2004 Oct 8;75(21):2505-13.
12. Zibadi S, Rohdewald PJ, Park D, Watson RR. Reduction of cardiovascular risk factors in subjects with type 2 diabetes by Pycnogenol supplementation. Nutr Res. 2008 May;28(5):315-20.
13. Liu X, Zhou HJ, Rohdewald P. French maritime pine bark extract Pycnogenol dose-dependently lowers glucose in type 2 diabetic patients. Diabetes Care. 2004 Mar;27(3):839.
14. D'Andrea G. Pycnogenol: a blend of procyanidins with multifaceted therapeutic applications? Fitoterapia. 2010 Oct;81(7):724-36.
15. Singh U, Jialal I. Alpha-lipoic acid supplementation and diabetes. Nutr Rev. 2008 Nov;66(11):646-57. doi: 10.1111/j.1753-4887.2008.00118.x. Review. Retraction in: Nutr Rev. 2012 Aug;70(8):482.
16. Harding SV, Rideout TC, Jones PJ. Evidence for using alpha-lipoic acid in reducing lipoprotein and inflammatory related atherosclerotic risk. J Diet Suppl. 2012 Jun;9(2):116-27.
17. Mijnhout GS, Alkhalaf A, Kleefstra N, Bilo HJ. Alpha lipoic acid: a new treatment for neuropathic pain in patients with diabetes? Neth J Med. 2010 Apr;68(4):158-62.
18. Ooi CP, Loke SC. Sweet potato for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2012 Feb 15;2:CD009128.
19. Unfer V, Carlomagno G, Dante G, Facchinetti F. Effects of myo-inositol in women with PCOS: a systematic review of randomized controlled trials. Gynecol Endocrinol. 2012 Jul;28(7):509-15.
20. Croze ML, Soulage CO. Potential role and therapeutic interests of myo-inositol in metabolic diseases. Biochimie. 2013 Jun 10. doi:pii: S0300-9084(13)00158-2. 10.1016/j.biochi.2013.05.011. [Epub ahead of print]
21. Dong JY, Xun P, He K, Qin LQ. Magnesium intake and risk of type 2 diabetes: meta-analysis of prospective cohort studies. Diabetes Care. 2011 Sep;34(9):2116-22. doi: 10.2337/dc11-0518.
22. Song Y, He K, Levitan EB, Manson JE, Liu S. Effects of oral magnesium supplementation on glycaemic control in Type 2 diabetes: a meta-analysis of randomized double-blind controlled trials. Diabet Med. 2006 Oct;23(10):1050-6.
23. Khan H, Kunutsor S, Franco OH, Chowdhury R. Vitamin D, type 2 diabetes and other metabolic outcomes: a systematic review and meta-analysis of prospective studies. Proc Nutr Soc. 2013 Feb;72(1):89-97.
24. Thomson RL, Spedding S, Buckley JD. Vitamin D in the aetiology and management of polycystic ovary syndrome. Clin Endocrinol (Oxf). 2012 Sep;77(3):343-50.
25. Sung CC, Liao MT, Lu KC, Wu CC. Role of vitamin D in insulin resistance. J Biomed Biotechnol. 2012;2012:634195.
26. George PS, Pearson ER, Witham MD. Effect of vitamin D supplementation on glycaemic control and insulin resistance: a systematic review and meta-analysis. Diabet Med. 2012 Aug;29(8):e142-50.
27. Thomas GN, Scragg R, Jiang CQ, Chan W, Marz W, Pilz S, Kim HC, Tomlinson B, Bosch J, Lam TH, Cheung BM, Cheng KK. Hyperglycaemia and vitamin D: a systematic overview. Curr Diabetes Rev. 2012 Jan;8(1):18-31.
This article originally featured in The September/October 2013 issue of Nutrition I-Mag.
Tags: Diabetes, Insulin Resistance, Metabolic Syndrome, Cinnamon, Magnesium, Lipoic Acid, Vitamin D, Inositol